Marijuana Rescheduling: What It Means for Policy, Patients, and the Industry
Recent developments have sparked debate among former DEA heads and White House drug czars over a potential move to reclassify marijuana from Schedule I to Schedule III, a step recommended by HHS. Supporters say rescheduling could ease research and taxes; critics warn it could “supersize” the industry. We break down the claims, counterpoints, and what it means for care via telemedicine in Virginia.
Background: What is Rescheduling?
Rescheduling marijuana means reclassifying it under the Controlled Substances Act (CSA), moving it from Schedule I (highest level of restriction, “no accepted medical use and high potential for abuse”) to a less restrictive schedule—or even removing it entirely from the CSA.
That change reflects evolving scientific understanding, shifting public opinion, and mounting pressure from policymakers and stakeholders who argue that the current federal designation is inconsistent with available medical research and the state-level legalization movements.
Why Rescheduling Matters: Industry Impacts
Banking, Finance, and Capital Markets
One of the biggest hurdles for the cannabis industry today is limited access to banking services. Because marijuana remains a Schedule I substance federally, many banks and financial institutions steer clear of cannabis businesses, forcing them to rely heavily on cash, informal financing, or gray-market lenders.
Rescheduling—or better yet, descheduling—would likely ease these constraints significantly. Businesses could open checking and savings accounts without fear of federal enforcement. They could access credit, lines of business lending, and other financial instruments more easily. Investment dollars might surge as institutional investors become less hesitant to enter a federally regulated but lower‐risk market.
Research and Development
Under Schedule I, researchers face major hurdles: tight federal oversight, limited supply channels, and the need for onerous approvals to study cannabis or its components. Rescheduling would reduce administrative barriers, simplify the process of obtaining research approvals, and broaden the legal supply of cannabis for scientific studies.
That means better and faster research into cannabinoids, dosing, delivery methods, clinical trials, and long-term health outcomes—which in turn fuels innovation in medical products, consumer goods, and pharmaceutical-grade therapies.
Federal- versus State-Level Legal Landscape
Currently, there's a major awkwardness: many states allow medical or recreational marijuana, yet under federal law, possession, distribution, and financing remain criminalized at the highest level. Rescheduling would help align federal and state laws, reducing legal ambiguity for businesses, patients, and regulators.
It could lead to more consistent interstate commerce rules, clarity in licensing, and potentially new frameworks for federal oversight that support, rather than contradict, state policies.
Law Enforcement, Criminal Justice, and Social Equity
A lower federal scheduling designation—or descheduling altogether—would reduce federal criminal penalties associated with marijuana. This could significantly change how the Justice Department prosecutes marijuana-related offenses, especially nonviolent or low-level cases.
Rescheduling might also reduce the burden of enforcement on federal agencies, freeing them to prioritize more serious drug offenses. In parallel, reform advocates argue that legal changes should be accompanied by proactive social equity programs, expungement of past convictions, and reinvestment in communities disproportionately harmed by past drug enforcement policies.
Market Expansion and Consumer Access
If federal rescheduling lowers barriers, the cannabis market could expand rapidly. Businesses would gain greater freedom to advertise, partner with mainstream distribution channels, and sell products across state lines (depending on federal rules).
Consumers might see lower prices, broader product variety, and improved access to medical cannabis via pharmacies or mainstream retail outlets.
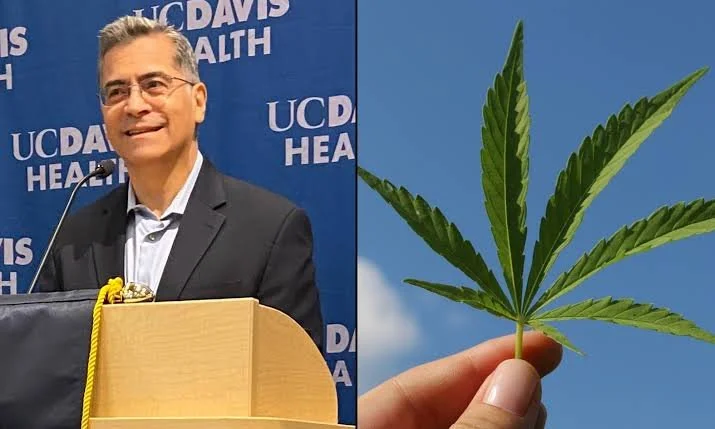
What the Experts Say: Former DEA and White House Voices
Prominent voices from within the DEA and former White House drug czars have publicly weighed in, warning the Biden administration to tread thoughtfully. Their core messages include:
Rescheduling should not be rushed — there are legitimate concerns about unintended consequences, including under-regulated markets, recreational misuse, and public health risks.
Coordination between federal and state agencies will be crucial to avoid chaotic transitions. Former officials emphasize the need for clearly designed regulatory and enforcement structures to prevent bad actors from abusing a looser federal designation.
Public health monitoring and oversight must accompany legal changes to mitigate risks and inform policy adjustments.
Transparency and incremental reform are preferable to sweeping changes without robust planning and stakeholder input.
In short, experts support reform—but urge caution, strong regulatory guardrails, and phased implementation.
Read Also: House Approves Psychedelic Research And Marijuana Labeling Amendments As Part Of Spending Bills
Telemedicine’s Role in a Rescheduled Landscape
As federal barriers ease, telemedicine—including telehealth platforms that prescribe or recommend cannabis-based medical treatments—could play a growing role in patient access and industry innovation. Here are key considerations:
Improved patient access: Telemed can reach patients in underserved or rural areas, providing consultations, follow-ups, and guidance without requiring in-person clinic visits. If federal regulations relax, more medical professionals might feel comfortable incorporating cannabis into their telehealth services.
Integration with broader health care: Rescheduling could allow cannabis to be prescribed, monitored, or recommended more like other controlled medications. Telemedicine providers could integrate cannabis treatment plans with other aspects of patient care (e.g., pain management, chronic disease, mental health), improving holistic outcomes.
Data collection and outcomes tracking: Telehealth systems can facilitate real‐time patient monitoring and feedback, enabling better data collection on efficacy, side effects, dosing strategies, and long-term outcomes. This can support both clinical research and continuous quality improvement.
Regulatory compliance, training, and standardization: As federal rules evolve, telemedicine providers will need to navigate licensure, prescribing regulations, and standards of care for cannabis. Early movers that build compliant, high-quality services may establish trusted reputations and gain market share.
In short, telemedicine could serve as a bridge between evolving federal policy and real-world patient and industry demand.
Challenges and Cautions
While rescheduling is widely seen as a net positive for the cannabis industry, it’s not a silver bullet. Key challenges include:
Regulatory complexity: Changing federal drug scheduling doesn’t automatically resolve state–federal conflicts, international treaty obligations, or diverse state laws. Federal agencies will need to develop detailed regulatory frameworks around licensing, product safety, interstate commerce, advertising, banking, and more.
Public health concerns: A looser schedule may increase access, but it may also increase misuse or use by vulnerable populations (e.g., minors, pregnant people). Regulators must monitor and manage risks such as impaired driving, mental health impacts, youth exposure, and diversion into illicit markets.
Uneven market outcomes: Without strong social equity safeguards, larger and better‐capitalized companies may dominate, leaving smaller businesses, minority-owned enterprises, and local producers behind.
Enforcement gaps during transition: During a policy shift, enforcement inconsistencies may persist. Some federal agencies might reduce prosecutions, while others (or states) might continue enforcement under older statutes, creating confusion or unfair disparities.
Stigma and policy inertia: Even if federal law changes, cultural attitudes, industry caution, and slow-moving regulatory agencies may delay the practical benefits of reform. Some stakeholders will resist change or demand stricter oversight, slowing implementation.
What’s Next and What Stakeholders Should Do
Policymakers and Regulators
Pursue phased and transparent reform: Gradual or tiered rescheduling—with clear benchmarks, oversight mechanisms, and opportunities for course correction—can help balance innovation with public safety.
Strengthen coordination and clarity between federal agencies, and between federal and state regulators, to ensure consistent policy and reduce unintended consequences.
Prioritize public health surveillance and create real-time monitoring systems for outcomes, misuse, and equity benchmarks.
Incorporate social equity safeguards into licensing, capital access, and market design—especially in states or regions disproportionately harmed by past cannabis enforcement.
Industry Players and Investors
Prepare for increased transparency and regulation: Even if restrictions loosen, federal oversight is likely to increase in parallel, so responsible actors should build robust compliance, quality-control, and data-tracking systems now.
Invest in research, product innovation, and telemedicine integration: Companies that position themselves early on evidence-based medical applications, delivery systems, and telehealth integration may gain advantages in a rescheduled market.
Advocate constructively for policies that promote fair competition, small-business access, and patient-centered models. Engaging with regulators, patient groups, and public health stakeholders can help shape reform in ways beneficial to all involved.
Use telemedicine to expand access and collect real-world data: Telehealth services can help build patient trust, scale medical cannabis access, and generate data to inform both product development and regulatory decision-making.
Final Thoughts
Rescheduling marijuana at the federal level represents a potentially transformative shift—not only for the cannabis industry, but for public health, criminal justice, and telemedicine. While the opportunities are substantial—from increased capital access and accelerated research to improved patient care and broader market growth—the transition must be managed carefully.
Former DEA leaders and White House drug czars rightly warn against rushing into reform without planning, regulatory guardrails, or monitoring systems. At the same time, platforms such as telemedicine are uniquely positioned to help bridge the gap between policy change and real-world patient and industry needs—if stakeholders act proactively, responsibly, and collaboratively.
As rescheduling advances from proposal to policy, the path forward will depend not just on legislative or regulatory changes, but on how stakeholders across the health, business, and public sectors adapt, innovate, and hold each other accountable.
FAQ
-
The possibility of federal employees using marijuana if it were rescheduled is complex and uncertain. While rescheduling may open up avenues for medicinal use under certain circumstances, federal agencies maintain strict drug policies, and marijuana's federal classification as a Schedule I substance presents legal and regulatory challenges. Each case would likely be evaluated individually, taking into account factors such as workplace safety, medical necessity, and adherence to agency-specific guidelines.
-
Currently, there are no FDA-approved medications derived directly from marijuana available for federal employees' use. However, medications containing synthetic cannabinoids, such as dronabinol (Marinol), are classified as Schedule III substances and are FDA-approved for medical use. Federal employees may use these medications under medical supervision, provided they adhere to agency-specific guidelines and disclose their medication use as required.
-
The inconsistency between state and federal regulations on marijuana creates legal gray areas, particularly for federal employees operating in states with legalized marijuana. While some states have legalized medical marijuana, federal law still prohibits recreational use and maintains marijuana's Schedule I classification. Federal employees are subject to strict drug policies, including mandatory drug testing for certain positions, which may conflict with state laws and individual healthcare needs. As a result, navigating the intersection of state and federal regulations poses challenges for federal employees regarding marijuana use and employment.