The History of THC: From Discovery to Medical Breakthroughs
Introduction
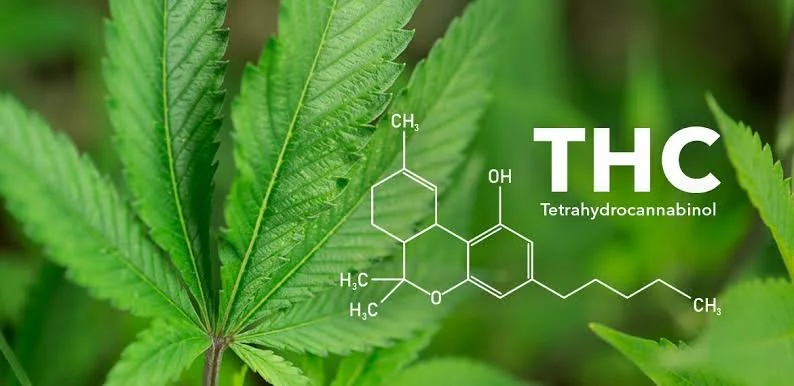
Tetrahydrocannabinol, more commonly known as THC, is the most well-known and psychoactive compound in cannabis. As the primary agent responsible for the plant's euphoric effects, THC has a long and complex history, starting from its early usage in ancient civilizations to its modern-day recognition as a potential treatment for a wide variety of medical conditions.
In this article, we will walk you through the journey of THC from its discovery to the numerous medical breakthroughs that have solidified its place in the realm of medical science.
Read Also: The Science Behind Microdosing THC: Benefits and Best Practices
Ancient Uses of Cannabis: Before THC Was Isolated
The use of cannabis dates back thousands of years, well before the active ingredient THC was identified. Archaeological evidence suggests that cannabis was first used by ancient cultures for its medicinal, spiritual, and recreational purposes. The earliest documented use of cannabis can be traced back to China around 2700 BCE. It was listed in the ancient Chinese pharmacopeia as a treatment for conditions such as pain, rheumatism, and malaria. In ancient India, cannabis was also used as a medicinal and spiritual substance, often incorporated into religious rituals and medical texts like the Atharva Veda.
While these ancient cultures understood that cannabis could have powerful effects, they had no knowledge of THC, the specific compound responsible for the plant’s psychoactive properties. Cannabis was used in various forms—usually in whole plant extractions—without any understanding of the individual chemical compounds at work.
The Discovery of THC: 1964 and Raphael Mechoulam
THC was officially discovered in 1964 by Dr. Raphael Mechoulam, an Israeli chemist who is often credited as the father of cannabis research. Working at the Hebrew University of Jerusalem, Mechoulam and his team were the first to isolate and identify THC as the primary psychoactive compound in cannabis.
Mechoulam’s discovery was groundbreaking. By isolating THC, he not only pinpointed the chemical responsible for the euphoric effects of marijuana but also paved the way for the exploration of how this compound interacts with the human body. This discovery set in motion decades of research into how THC affects both the mind and body, as well as its potential for medical use.
One of the significant contributions of Mechoulam's research was the identification of THC’s interaction with the endocannabinoid system (ECS), a biological system that plays a critical role in maintaining the body’s homeostasis. The ECS consists of a network of receptors, endocannabinoids, and enzymes that regulate various bodily functions, including mood, appetite, sleep, and immune responses. THC’s ability to bind to these receptors is what causes its psychoactive and therapeutic effects.
The Role of THC in the War on Drugs: Criminalization and Legal Challenges
In the mid-20th century, as cannabis use grew in popularity in the United States and other Western countries, the perception of the plant began to shift. What was once considered a medicinal plant became a target of regulation and criminalization. The Marihuana Tax Act of 1937 effectively made cannabis illegal in the U.S., setting the stage for a decades-long stigma against its use. Despite growing interest in THC’s potential medicinal properties, cannabis was classified as a Schedule I drug under the Controlled Substances Act of 1970, meaning it was deemed to have no medical value and a high potential for abuse.
This classification made research into THC difficult, as the legal framework limited access to the plant for scientific study. Despite these obstacles, some researchers persisted, and by the 1980s and 1990s, a growing body of evidence suggested that THC might offer valuable medical benefits for a variety of conditions.
Medical Breakthroughs: THC and the Treatment of Disease
The medical potential of THC was first seriously considered in the 1970s when researchers discovered that it could be used to treat glaucoma, a condition characterized by increased pressure in the eyes. Studies showed that THC could reduce this pressure, offering an alternative treatment for patients who were unresponsive to traditional therapies. This was one of the first instances where THC was recognized for its therapeutic potential in the medical community.
However, it wasn’t until the 1980s that THC made its most significant medical breakthrough. During the height of the AIDS crisis, patients began using cannabis to manage the debilitating side effects of the disease and its treatments. THC was found to be effective in stimulating appetite and reducing nausea, both of which were critical for patients undergoing treatments that caused significant weight loss and malnutrition. These effects were eventually supported by clinical studies, leading to the approval of Marinol (dronabinol), a synthetic form of THC, by the U.S. Food and Drug Administration (FDA) in 1985. Marinol became one of the first cannabis-based medications legally available for prescription, primarily for treating nausea and vomiting in chemotherapy patients.
Read Also: The Role of THC in Treating Chronic Pain
THC and Pain Management: A Growing Field of Research
As research into THC continued, one of the most promising areas of study was in pain management. THC's interaction with the endocannabinoid system, particularly its activation of CB1 receptors in the brain, was found to help reduce the sensation of pain. This discovery was especially significant for patients suffering from chronic pain conditions, such as those caused by multiple sclerosis, arthritis, and neuropathic pain.
Cannabis, with its high THC content, became a valuable alternative for patients who were either resistant to traditional pain medications or seeking alternatives to opioids. Given the opioid crisis in the U.S. and around the world, THC’s role in pain management became increasingly important as a less addictive option for patients dealing with chronic pain.
Read More: Top 5 THC Drinks
THC in Neurological Conditions: Seizures and Epilepsy
One of the most widely publicized medical applications of THC (and cannabis in general) has been in the treatment of epilepsy and seizure disorders. THC and CBD, another major cannabinoid, have both been found to reduce the frequency and severity of seizures in some patients, particularly those with treatment-resistant forms of epilepsy such as Dravet syndrome.
While CBD has been the focus of most of the epilepsy research, THC’s role cannot be discounted. Some studies have shown that a combination of THC and CBD offers a more effective treatment than CBD alone. In 2018, the FDA approved Epidiolex, the first cannabis-based medication containing CBD, for the treatment of seizures, which further fueled interest in how THC might be used in neurological conditions.
Related: Do THC Suppositories Really Work?
Modern-Day Legalization and THC’s Place in Medicine
The 21st century has witnessed a seismic shift in the perception of cannabis and THC. As more states in the U.S. and countries worldwide have moved toward the legalization of medical and recreational cannabis, THC has become a central focus of research and public debate. Medical marijuana programs in states like California, Colorado, and New York have allowed patients to access THC-rich strains for the treatment of various conditions, from chronic pain to post-traumatic stress disorder (PTSD).
Research into THC’s medical applications is expanding, with ongoing studies investigating its potential in treating conditions such as Alzheimer’s disease, Parkinson’s disease, and cancer. THC's anti-inflammatory, pain-relieving, and neuroprotective properties continue to make it a valuable compound in the search for new medical treatments.
The Future of THC in Medicine
As the legal landscape surrounding cannabis continues to evolve, the future of THC in medicine looks promising. With more research opportunities and clinical trials, scientists are uncovering new ways that THC can be used to treat a variety of health conditions. Beyond just recreational use, THC is increasingly being recognized as a powerful tool in the management of chronic diseases and symptoms that are often difficult to treat with conventional medications.
Conclusion
The history of THC is a fascinating journey from its ancient use in medicinal practices to its current status as a potential treatment for a wide range of conditions. From Raphael Mechoulam's discovery in 1964 to the ongoing medical breakthroughs in modern times, THC has come a long way in changing how we view cannabis as a therapeutic substance. As research continues, the full extent of THC’s potential in medicine is likely to unfold, offering new hope for patients around the world.
FAQ
-
The first FDA-approved THC-based medication was Marinol (dronabinol) in 1985. It is a synthetic form of THC used to treat nausea and vomiting caused by chemotherapy and stimulate appetite in patients with AIDS.
-
THC has shown effectiveness in managing chronic pain conditions such as arthritis, multiple sclerosis, and neuropathic pain. It interacts with the body's pain receptors, providing relief and acting as an alternative to opioids.
-
THC is being used to treat conditions such as glaucoma, epilepsy, PTSD, chronic pain, and nausea associated with cancer treatments. Ongoing research also explores its potential in treating Alzheimer’s, Parkinson’s disease, and certain forms of cancer.