Cannabis vs. Alcohol: A 2026 Physician Survey of 1,000 Patients
Article Key Takeaway
In 2026, I conducted a physician-led survey of 1,000 medical cannabis patients to better understand how medical cannabis use influenced alcohol consumption and overall quality of life. What I discovered was both unexpected and clinically significant.
The findings highlight the value of physician-directed research using anonymized patient data to uncover real-world behavioral shifts. A striking majority of patients reported reducing their alcohol intake after beginning medical cannabis treatment, despite not intending to do so. This pattern aligns with broader public health research describing the “substitution effect,” where individuals replace higher-risk substances with lower-risk alternatives. In fact, latest surveys show that three in four young adults use marijuana as an alcohol alternative at least once a week.
The contrast in safety profiles is difficult to ignore. Alcohol is associated with more than 178,000 deaths annually in the United States and carries well-documented toxicity risks. Medical cannabis, when used under physician supervision, does not share the same lethal toxicity profile and may offer a safer pathway for patients seeking long-term symptom management.
In this article, I share the full data from my 1,000-patient survey, and what it may signal about an evolving public health shift already underway.
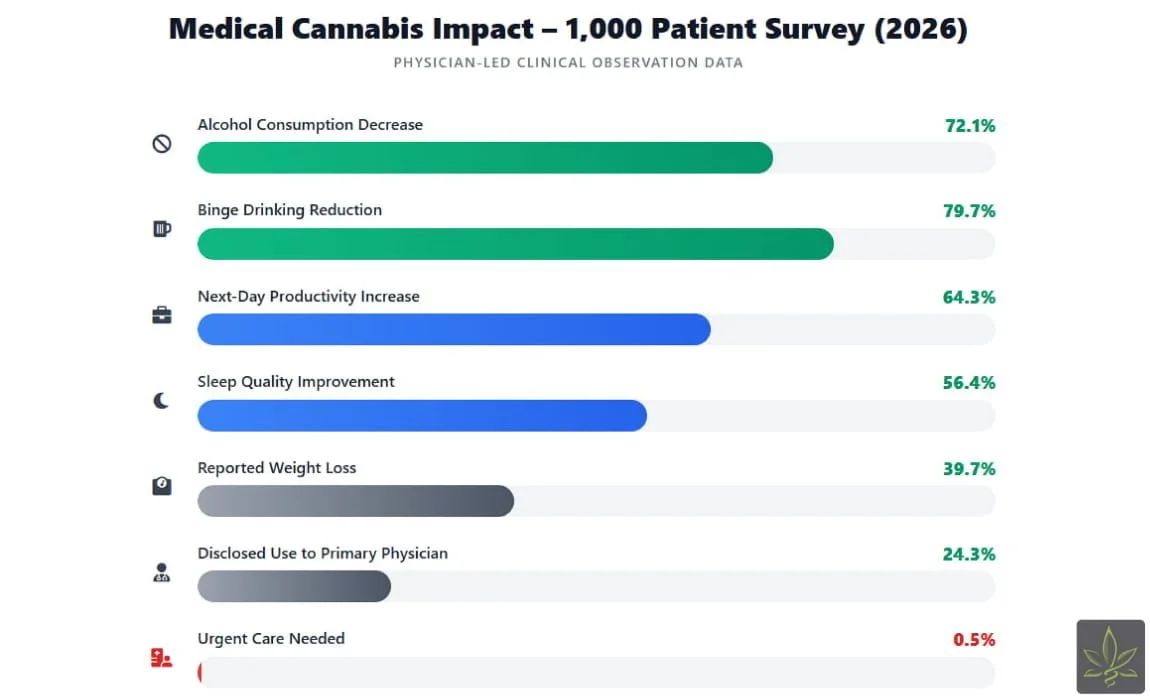
Key Data Insights from Study
Alcohol Reduction: 721 out of 1,000 patients (72.1%) reported a decrease.
Binge Drinking: 44 of the 55 patients who tracked binge drinking episodes reported a reduction in binge drinking episodes.
Productivity: 643 patients (64.3%) reported increased next-day productivity.
Sleep: 564 patients (56.4%) noticed improved sleep quality.
Safety: Only 5 patients (0.5%) reported an urgent care visit related to cannabis.
Disclosure Gap: 759 patients (75.9%) have not disclosed their use to their primary physician, primarily citing "Fear of Stigma."
See how much you could save with a medical card
Introduction: The Accidental Wellness Shift
When I began reviewing the data from 1,000 patients in my care, I was not expecting alcohol to become the headline. Most patients entered medical cannabis treatment for chronic pain, anxiety, sleep disorders, PTSD, or inflammatory conditions. Alcohol reduction was not the stated goal.
Yet in our testing and follow-up surveys, 72.1% reported that their alcohol consumption decreased after initiating physician-guided medical cannabis.
Even more compelling: among patients who had previously engaged in binge drinking, 79.7% reported a reduction in binge episodes.
I struggled, initially, to understand whether this was coincidence or causation. But as I cross-referenced our internal findings with peer-reviewed literature, including substitution research published in the Harm Reduction Journal, the alignment became increasingly difficult to ignore. That study documented that many medical cannabis patients reported intentionally or unintentionally reducing their alcohol consumption after initiating cannabis treatment.
Seeing similar patterns emerge independently within my own 1,000-patient dataset suggested that what we were witnessing was not random variation, but part of a broader, documented behavioral shift consistent with the substitution effect.
For many patients, the shift wasn’t ideological. It was functional. They felt better. They slept better. They performed better the next day. And without intending to, they drank less.
Data Overview: Physician-led 1,000 Patient Survey
| Survey Question / Metric | Patient Response / Data Point |
|---|---|
| Did your alcohol consumption change after starting medical cannabis? | 72.1% Reported a Decrease |
| Was alcohol reduction your primary intention when first using cannabis? | 96.1% No (Primary goals were pain, anxiety, sleep, or other) |
| Did you experience a reduction in "Binge Drinking" episodes? | 79.7% of Binge Drinkers Reported a reduction |
| How has your next-day productivity changed since the transition? | 64.3% Reported an Increase |
| Did you notice an improvement in your quality of sleep? | 56.4% Reported Significant Improvement |
| Have you noticed any changes in your body weight? | 39.7% Noticed Weight Loss |
| Have you ever required urgent care due to medical cannabis use? | 0.5% Yes (Less than 1%) |
| Have you disclosed your cannabis use to your primary care physician? | 24.3% Yes |
| Main reason for NOT disclosing cannabis use to a doctor? | Fear of being Stigmatized |
72.1% Reported a Decrease in Alcohol Consumption
This was the number that truly stopped me.
Nearly three out of four patients in my survey reported reducing their alcohol intake after beginning medical cannabis treatment, even though 96.1% of them did not start cannabis with the goal of drinking less. That detail matters. This was not a sobriety program. It was not an anti-alcohol initiative. It was a medical treatment plan for pain, anxiety, insomnia, inflammation, and other chronic conditions.
Yet alcohol consumption dropped.
In reviewing patient responses, I noticed something consistent. The reduction wasn’t forced. It wasn’t dramatic. It was quiet and gradual. Patients would say things like, “I just don’t feel the need to drink anymore.” Others described fewer drinks per week, no weekend binges, or replacing nightly wine with a low-dose tincture.
The shift was functional. When symptoms improved, alcohol became less relevant.
79.7% of Binge Drinkers Reported a Reduction
When I analyzed the subset of patients who previously tracked binge drinking episodes, I was surprised with what it was telling me.
But the pattern was clear.
79.7% of patients who identified as binge drinkers reported reducing their binge drinking episodes. This is a measurable transformation that provides real benefits in their lives..
In reviewing individual patient feedback, I noticed a common thread: once anxiety levels stabilized and sleep improved under physician-guided cannabis care, the triggers that previously led to binge drinking began to diminish. Patients described feeling more emotionally regulated, less impulsive, and more controlled in social settings.
64.3% Reported Increased Next-Day Productivity
One of the strongest themes in our survey was productivity.
64.3% of patients reported feeling more productive the next day after transitioning away from alcohol. This was especially noticeable among working professionals, teachers, nurses, executives, business owners, who described waking up clearer and more focused.
In clinic conversations, patients often contrasted their experiences directly. With alcohol, they described sluggish mornings, brain fog, and low motivation. With regulated, physician-guided cannabis use, particularly low-dose evening formulations, they described steadier sleep and clearer mornings.
Cannabis is not without psychoactive properties. That is why dosing and timing matter. In our cohort, many patients were not using cannabis to intoxicate. They were using it therapeutically, intentionally, conservatively, and under guidance.
The difference showed up the next day.
56.4% Reported Significant Improvement in Sleep
Sleep improvements were another consistent finding.
More than half of patients reported meaningful improvements in sleep quality after reducing alcohol and initiating cannabis therapy. In my clinical experience, many patients initially rely on alcohol as a sleep aid. It may help them fall asleep, but it rarely sustains restful sleep throughout the night.
When we transitioned patients to carefully titrated cannabis regimens, often focused on evening dosing, they frequently reported deeper, more sustained rest. Fewer awakenings. Less early-morning fatigue.
Improved sleep, in turn, appeared to influence other areas: mood stability, impulse control, productivity, and alcohol reduction itself.
It became clear that sleep was not an isolated metric. It was part of a larger wellness shift.
39.7% Reported Weight Loss
This was one of the more unexpected findings.
39.7% of patients reported weight loss after reducing alcohol and continuing medical cannabis treatment. In reviewing their feedback, many attributed this change to eliminating nightly drinks, reduced late-night snacking associated with alcohol use, and improved energy for physical activity.
The weight changes were generally modest but consistent over time. Six to twelve months into treatment, patients reported steady progress rather than rapid swings.
Interestingly, appetite stimulation, often associated with cannabis, did not appear to drive weight gain in this cohort. Instead, the reduction in alcohol consumption seemed to play a more significant role.
Only 0.5% Required Urgent Care
In a group of 1,000 patients, five reported requiring urgent care related to cannabis use.
When I reviewed those cases, most involved dosing errors in inexperienced users, particularly those who self-adjusted without consultation. These were not cases of toxicity. They were cases of unintentional overdose
This distinction is important.
No medication is risk-free and cannabis is no exception to that rule. However, compared to the number of emergency room visits reported annually related to alcohol it appears cannabis use requires less frequent emergency room visits.
From a safety standpoint, physician oversight clearly matters. Structured dosing, education, and follow-up reduce risk significantly.
The Disclosure Gap: 75.9% Do Not Tell Their Primary Physician
This may be the statistic that concerns me most.
75.9% of patients reported not disclosing their cannabis use to their primary care physician. The most common reason was fear; fear of being judged, labeled, or stigmatized.
Even though these patients were using cannabis legally and under medical supervision, they still hesitated to share that information with their broader care team.
As a physician, that troubles me deeply.
Medicine functions best when communication is transparent. Coordinated care improves safety. If patients feel uncomfortable disclosing legal, physician-guided treatment, then stigma remains embedded in our healthcare culture.
This disclosure gap represents societal views on cannabis and its perceived benefit as a legitimate medication.
The Bigger Picture: What I Observed
When I stepped back from the individual data points, a broader pattern emerged.
This was not just about cannabis. It was about behavior, wellness, and substitution. Patients were not simply switching substances. They were shifting toward something they believed offered them better results with fewer side effects.
Alcohol use declined, binge drinking episodes dropped, sleep improved, productivity increased, a significant percentage reported weight loss urgent care visits were rare, and yet, stigma remained.
From where I stand as a physician, this shows there may be significant benefits to medical cannabis, however more studies must be conducted under more controlled environments.
The shift I observed in these 1,000 patients was not intentional but most patients welcomed the results
It suggests that when patients receive structured, physician-guided cannabis care, numerous benefits could result.
What I Learned as a Physician
When I began this survey, I wasn’t sure what I expected to see. I had read other studies and articles that pointed to cannabis use resulting in alcohol reduction but what I found went beyond alcohol reduction..
Patients weren’t to reduce their alcohol use in most cases.. They were seeking relief from pain, insomnia, and anxiety. The alcohol reduction was a byproduct.
I call it the Accidental Substitution Effect because it was rarely planned.
In medicine, we often debate policy in theory. But in examining anonymized patient data firsthand, I saw a real-world trend that warrants further study.
This is not an endorsement of recreational use and I am not saying cannabis use does not have its downsides if not used appropriately.
When patients are offered regulated, physician-guided cannabis options through a state-issued medical card, many voluntarily reduce alcohol consumption, and report measurable improvements in productivity, sleep, and overall quality of life.
Final Thoughts
When I began reviewing this data, my main goal was to better understand my patients and see how cannabis for better or worse altered their lives.
As physicians, we are trained to weigh risk profiles, long-term outcomes, and quality-of-life indicators. Alcohol’s risks are well documented in public health literature, from liver disease to cardiovascular complications and injury. Cannabis, while not without side effects, presents a dramatically different toxicity profile when used responsibly under medical supervision.
What stood out most in this survey was how much cannabis helped patients reduce their alcohol intake.. Patients reported fewer binge episodes, better sleep, clearer mornings, and improved productivity. They weren’t chasing intoxication, they were seeking medical treatment.
But data alone is not enough. The real safeguard is physician oversight, proper dosing, formulation selection, medical history review, and ongoing monitoring. Substitution without guidance can create new risks; substitution with structured medical supervision can create measurable improvements.
At CannabisMD TeleMed, we work alongside the physicians on our platform to conduct ongoing research and provide structured, compliant evaluations that prioritize safety, transparency, and long-term wellness. This is precisely why we do everything possible to ensure that patients in need of medical cannabis treatment can receive a comprehensive consultation and the necessary certification to purchase from regulated dispensaries. Based on our experience, once patients transition to this professional framework and receive individualized guidance, clinical outcomes improve and the weight of social stigma significantly decreases.
If this survey tells us anything, it is this: healthcare conversations are evolving. The responsible path forward is not silence, stigma, or self-experimentation. It is physician-guided care through state approved medical cannabis programs in conjunction with healthcare practitioners.. As more patients choose that path, we will continue to document what we see while preserving patient anonymity.
Resources
Deaths from Excessive Alcohol Use in the United States. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/mmwr/volumes/73/wr/mm7308a1.htm
Substitution of cannabis for alcohol, prescription medications, and other substances: A survey of 973 medical cannabis patients. Harm Reduction Journal (National Library of Medicine). https://pubmed.ncbi.nlm.nih.gov/28115712/
Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach. Scientific Reports (Nature). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4311234/
The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies of Sciences, Engineering, and Medicine. https://nap.nationalacademies.org/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state
Cannabinoids, Endocannabinoids, and Sleep. National Institutes of Health (NIH) / PubMed Central. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3836309/
Prevalence of Marijuana Use Among U.S. Adults With Pain, Anxiety, or Depression. JAMA Network Open. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2788241
Frequently Asked Questions
-
Once you begin your medical cannabis journey, we strongly advise against "cross-fading" or simultaneous use. On our platform, physicians often observe that combining the two can lead to "additive impairment," significantly increasing dizziness and nausea.
-
This is a primary concern for the 75.9% of patients who fear stigma. On our platform, we maintain strict HIPAA compliance. Your evaluation is a private medical record. While a medical card protects your status as a patient in states like Virginia or Pennsylvania, it is important to note that workplace drug testing protections and policies vary by state and employer. Once you have your certification, we recommend reviewing your specific corporate handbook and state’s medical cannabis legislation, as a medical card does not always grant immunity from private company drug policies.
-
In my clinical experience, the dependency profiles are fundamentally different. Alcohol withdrawal can be life-threatening and often requires clinical detox. While Cannabis Use Disorder (CUD) is a very real risk, the physical withdrawal is typically reported as mild - comparable to caffeine or nicotine cessation. By following a physician-guided dosing schedule, you can minimize the risk of addiction while maximizing therapeutic benefits.